How can ECSTASY help with trauma?
From the dance floor to drug agency approval with talk of revolutionary therapy. Ecstasy to treat post-traumatic stress disorder!
On my Instagram (@Peto.BeWise), I asked you if you've ever tried ecstasy or MDMA. Not very surprisingly, about a third of you answered "yes". Ecstasy is, after all, one of the most popular "party" drugs today. However, only few have any idea that ecstasy has enormous potential in the treatment of one of the most severe psychiatric disorders - post-traumatic stress disorder. But first, let’s look at what ecstasy or MDMA is.
What is ecstasy or MDMA?
MDMA or chemically 3,4-methylenedioxymethamphetamine, is a white-yellow crystalline substance that belongs to the amphetamine group. In the scientific literature, MDMA is commonly referred to by the word 'ecstasy'. However, colloquially, a distinction is often made between the pure crystalline substance 'MDMA' and 'ecstasy', which refers to its adulterated tablet form. In this text, I will talk exclusively about pure MDMA.
You may have noticed the word methamphetamine in the chemical structure. You know, 'meth', 'speed', the horrible street drug! MDMA actually belongs to the same chemical group as methamphetamine. How do you normally picture a person under the influence of MDMA? He can't stay still, has endless energy and dances for hours. Amphetamines are truly one of the most powerful stimulants we know.
Not really a stimulant
However, if I left the definition of MDMA at "it's a stimulant like other amphetamines", experts on the subject wouldn't be very happy. Indeed, MDMA is a drug that sits between the stimulant and psychedelic categories without fully meeting the criteria of either. MDMA does cause stimulation of the body, but this is accompanied by euphoria and, at higher doses, almost psychedelic hallucinations. Most typical and most relevant to our story are its effects on our emotions. These are so characteristic that MDMA has been given its own category as an empathogen. An empathogen is a substance that dramatically increases empathy, affection and love for those around you. As one follower wrote to me on Instagram:
"I tried it once, and it stirred up all kinds of emotions in me. I didn't even know they existed. Absolute love and warmth for everyone and everything. A very powerful experience."
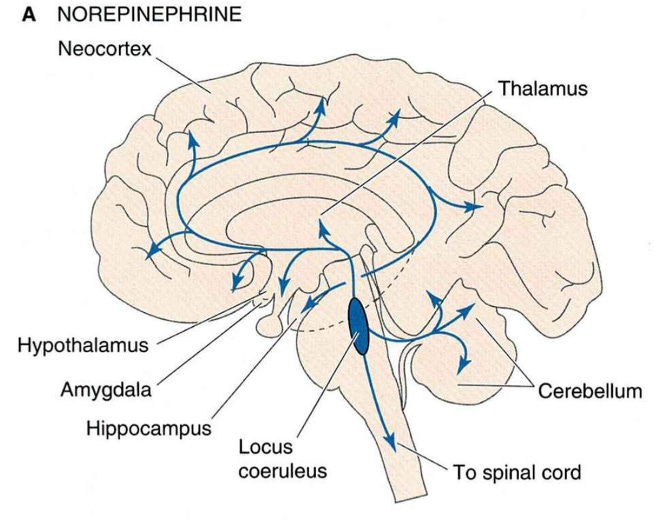
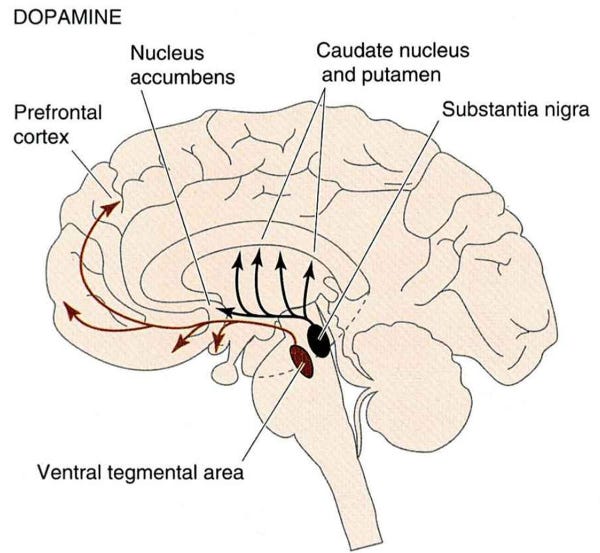
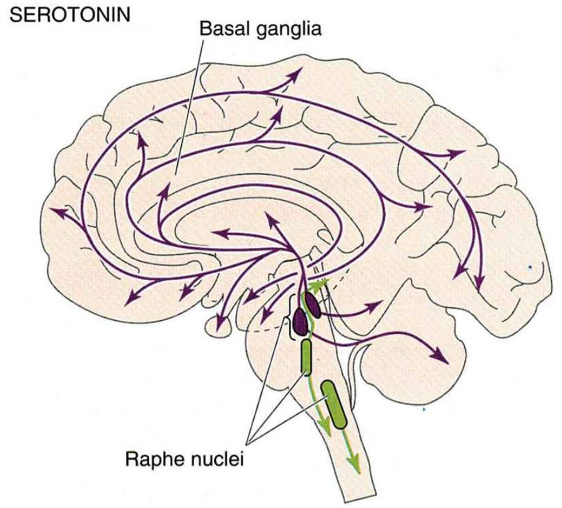
Both the physical and emotional dimensions of MDMA's effects can be fairly easily inferred from its workings on the brain. Our brains have a stalk-like structure sticking out of the base, which we call the brainstem. The brainstem contains three very important groups of neurons, which hug almost the entire brain with their projections (axons). We divide these three groups according to what chemical compound (neurotransmitter) they produce and secrete - norepinephrine, dopamine or serotonin. MDMA can affect all three groups of neurons, causing them to massively release their neurotransmitters. It also prevents the transport of neurotransmitters back into the neurons, which normally stops the signalling. In other words, not only do neurons secrete more neurotransmitters, but MDMA also greatly prolongs their action in the brain.
The physical side of the "high" is explained mainly by norepinephrine. You can think about norepinephrine as an 'on' switch of the brain. During sleep, norepinephrine neurons are almost inactive. When you wake up, their activity increases and they have their highest activity during alert states. When you're standing in front of a blackboard at school with your heart rate elevated and palms sweaty. When you are walking down an empty street in the evening and suddenly hear a strange sound behind you. You become alert, and your senses heighten. These are all situations in which the norepinephrine neurons fire the strongest.
The effect on the norepinephrine system is typical for all amphetamines. Also typical is the effect on the dopamine system. Dopamine is responsible for energising the body, feelings of motivation, and at high levels, is thought to induce euphoria. For example, a pleasant feeling of a job well done, exercise, enjoying food or having sex - that's the dopamine playing its role. Thus, it is the release of dopamine that is likely to account for the euphoric effects of MDMA.
Finally, the third neurotransmitter, serotonin, is the neurotransmitter that makes MDMA distinctly different from the rest of the amphetamines. MDMA preferentially increases serotonin rather than dopamine or norepinephrine, which is very atypical for amphetamines. In contrast, the effect on serotonin is characteristic of classical psychedelics such as LSD or psilocybin.
Massive serotonin release plays a role in the relaxing element of MDMA. Everything is fine, I feel calm, nothing is bothering me, and I feel peaceful. Serotonin has very typical anti-aggressive effects. Because of the serotonin release, we are friendlier, more open and more at peace with our circumstances.
Many therapists, looking at the profile of the mind under the influence of MDMA, have thought that ecstasy could be utilized for therapy. The first diagnosis that came to mind was post-traumatic stress disorder (PTSD). And soon, we will understand why.
When your body thinks it’s always in danger
Post-traumatic stress disorder, abbreviated as PTSD, is one of the most debilitating psychiatric disorders. Usually, we associate this disorder with war veterans who have experienced highly stressful and brutal situations. However, PTSD is also very common in the general population. Approximately 10% of victims of natural disasters and more than 40% of victims of sexual violence will encounter a diagnosis of PTSD.
PTSD is characterised by so-called "flashbacks", i.e. the sudden reliving of traumatic memories. These memories also return to a person's consciousness during sleep in the form of nightmares, which further impair the individual's mental health. Patients are usually distrustful of their surroundings, assume hostile attitudes of everyone around them and are constantly on alert. Simply put, their brain assumes danger at every turn. Bursts of aggression and the inability to feel joy or other positive emotions are also very common features of PTSD.
PTSD is very much a story of the body's excessive arousal and inadequate processing of memories. As we explained above, norepinephrine brainstem signalling is essential for our survival. Stress response helps to improve both cognitive and physical abilities. Stress is necessary and beneficial, but only in the short term and within a reasonable range. Once there is too much stress, it damages both the brain and the whole body.
Take the simple example I mentioned earlier. You are walking down a seemingly empty street at night. Suddenly you hear footsteps behind you. Norepinephrine neurons start working, your senses become sharp, your heart starts pumping, your muscles fill with blood. With your senses heightened, you instantly see the man with the knife coming towards you. Without thinking, you run and run faster than ever before. When you are safe, you calm yourself. And we are interested in what starts happening after the whole situation.
Your brain analyzes the situation and learns to recognize "cues" of the situation that preceded the danger. Doing so, you will be faster to turn on the stress response in the future and increase the chances of survival. For example, the brain remembers that you should be stressed if you are walking alone down a street during night. It also remembers that maybe you should be stressed when you are walking down that one particular street. However, the opposite process also happens. As long as you're healthy, your brain will correctly recognize that the stress response is not adequate when you're walking down the street on a white-out day when there are plenty of people. It will also correctly recognize that the stress response is inadequate when you are walking down any street or when you see any person walking down a street. It will form adequate and inadequate "cues" for when to turn on the stress response.
And this ability is severely impaired in PTSD patients. It is believed that the hyper-alert state of the brain during a very traumatic situation disrupts the proper incorporation of memory into a person's mind. The traumatic experience can not be broken down into adequate and inadequate cues. On the contrary, a general cue is encoded into the mind resulting in sending your body into a hyper-alert state even if relevant cues are missing. Or perhaps more accurately, everything seems to be a relevant cue. Thus, the war veteran expects an explosion, even when shopping for groceries. The brain is unable to distinguish and understand that the threat is no longer there and is specific to a particular situation and a particular cue.
It is believed that the high level of norepinephrine in the brain prevents the traumatic memory from being properly incorporated. Multiple studies have repeatedly shown that PTSD patients have increased activity of norepinephrine neurons both during the day and during sleep. Conversely, medications that can reduce norepinephrine levels have been shown to help alleviate symptoms such as nightmares. To simplify, to properly incorporate trauma, we need to create a state in the mind that does not expect an enemy at every turn. And so we finally come to how MDMA can help in treatment.
Is MDMA the penicillin of PTSD?
The psychotherapeutic approach used in the treatment of PTSD to date involves the conscious and repeated recall of traumatic memories. Together with the psychotherapist, the patient tries to relive the trauma in his or her mind, but this time in an environment that is safe and supportive. The logic is that by repeated exposure to the memory in a safe environment, the trauma can be properly decomposed into relevant and irrelevant cues. In a safe environment, the brain learns to recognise that it is not necessary to activate the alarm in every situation.
Although according to many studies, this approach works, the problem is that it works only in a very limited way. Only about two-thirds of all patients respond to treatment, and of those, more than half still meet the criteria for a PTSD diagnosis even after long-term therapy. This may be because it is simply too traumatic for patients to reinvoke a memory. The mind has created lots of defence mechanisms, and it's very hard to go around them. And this is where a tremendous help called MDMA comes in.
In defining MDMA, I mentioned that it increases norepinephrine levels in the brain. This doesn't go along with the information above that we need to lower norepinephrine levels for therapy. Therefore, I will remind you that MDMA is a very atypical stimulant, increasing serotonin to a much higher degree than dopamine or norepinephrine. This puts the mind into a peaceful, friendly and more open state. Indeed, from the testimonies of the first patients who have undergone MDMA-assisted therapy, it seems that the induced state of mind is crucial for the therapy. Here are a few of them:
Patient 1:
"It brings you euphoria and love. You can go into the dark and not be afraid."
Patient 2:
"I dreamt I was sitting at a big table in a comfortable chair. The drug materialized in physical form and brought me a folder with my personal records. It said I needed to look it over and talk to a therapist about it so it could be filed properly."
Patient 3:
"Under the influence of MDMA, I was able to talk about my trauma without having a physiological reaction. It sort of rewired the brain to a pre-PTSD baseline."
It is obvious MDMA doesn't work like a pill you take as an antibiotic, and suddenly you're better. The whole procedure is called MDMA-assisted therapy. And thus, one doesn't work without the other. MDMA creates a friendly environment of the mind into which the traumatic memory can be put to light. This makes the trauma easier to be explored and incorporated back into the mind in a healthy way. The result is an integrated memory that does not trigger an alarmed state, anxiety or nightmares.
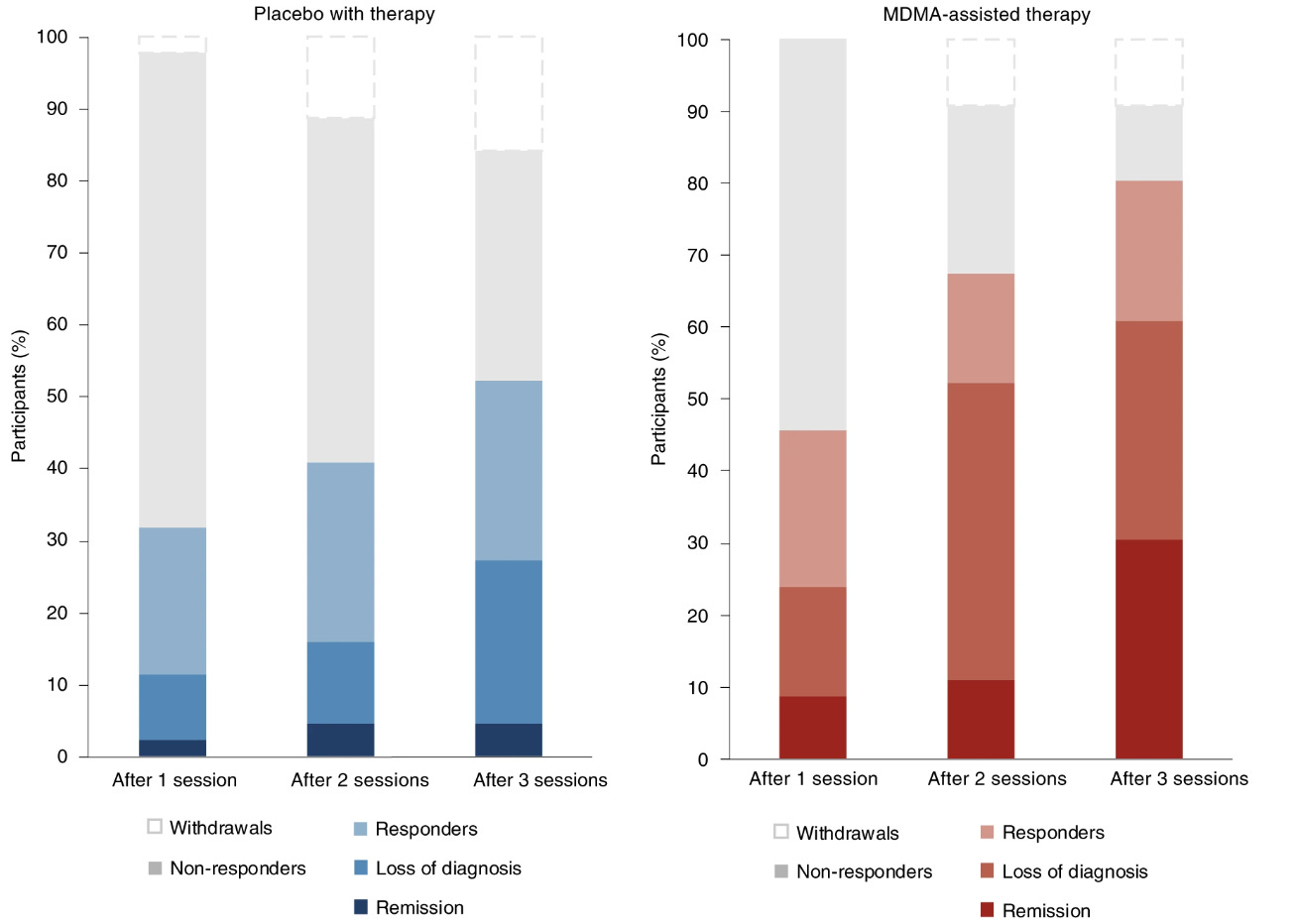
One of the largest studies found that after three therapy sessions, 67% of participants (28 of 42) in the MDMA group no longer met the criteria for PTSD compared to 32% of participants (12 of 37) in the placebo group. In addition, 33% of participants (14 of 42) in the MDMA group met remission criteria, while only 5% of participants (2 of 37) in the placebo group did (graph below).
It must be said that the 67% who no longer fell under a PTSD diagnosis are not fully recovered individuals. A diagnosis of PTSD involves multiple criteria, and you must meet at least a few of them to be diagnosed. In other words, these people weren't suddenly completely healthy, but they didn't meet the official criteria anymore. The closest to recovery is the remission category. But even there, a 33% difference in the MDMA group vs 5% in the placebo group is a huge accomplishment.
In early 2023, the Association for Psychedelics Research MAPS announced that they would publish another study this year that once again confirms the efficacy of MDMA-assisted therapy for the treatment of PTSD. This data will serve as evidence for FDA, to whom MAPS has submitted an application for approval of MDMA for assisted therapy. And according to some experts, we may see FDA approval as early as this year. The European EMA is expected to follow right after that.
From the dance floor to approval by drug agencies with claims about being a“revolutionary drug”. My online activities are specifically intended to demonstrate that these "drugs" are merely chemicals, and how we handle them is entirely up to us.